So this is my second in a series of transpartisan proposals, the unintended consequence of which is likely to have me ostracized not just by the two major parties but by the libertarian community as well. My first such proposal, on climate, helped get me ostracized from the climate skeptic community. Much of this article is based on a proposal I first made in 2015.
I want to say at the top that unlike my climate plan, this is not a plan so much as a concept for a plan. As in climate, tribalism and muddled thinking about goals has made it hard to make forward progress on the role of government in health care. The Democrats in 2008 and 2018 and the Republicans in 2010 arguably won a lot of Congressional seats stirring up fears about health care, so it is a vital issue with the public. For those who want to just dig in their heals and wait until it all goes away, I don't think this will happen. And I think the logic I outline is superior to the typical political process described by Megan McArdle as
- Something must be done.
- This is something.
- Therefore, this must be done.
I think the key to creating a viable program for health care depends on being very clear on the goals that one is trying to achieve and matching those goals well with the capabilities of government. Obamacare was a huge mess in this regard, weaving all over the place in terms of goals (increasing insurance coverage, lowering costs, improving care effectiveness) and assigning roles to the government that were laughably poorly matched to its skills.
Take increasing the percentage of Americans with health insurance, probably the number one goal of Obamacare and the metric most cited to evaluate its success. Is the core need of Americans really to have health insurance, or it something else? Is mandating that people buy insurance they don't value in order to improve this metric really improving individual well-being? Does increased coverage really translate to increased health? (spoiler -- any causal link here is really tenuous in the data). All these questions and more exist because increasing insurance coverage was the wrong goal. So is anything having to do with "pre-existing conditions" as Democrats framed it (fairly successfully) in the recent election.
The #1 Consumer Need and Fear in Health Care
Here is my main assumption: The real, core need of individuals is that a) when they or a family member get dreadfully sick, lack of money will not be a barrier to getting them the needed care and b) even if they can get the care, they would really prefer not to be bankrupted by it. All these other things -- percent covered by insurance, mandates to accept pre-existing conditions, insurance mandates and subsidies -- are all imperfect proxies for this core need.
This is exactly the kind of need that we buy catastrophic insurance to cover. I would be bankrupted and homeless if my house burned down and I was still responsible for the mortgage but relatively inexpensive fire insurance covers that. Losses are not usually correlated (ie one loss does not make it more likely I have a second loss, except in flood insurance which is why there is no private flood insurance any more) so I don't worry about non-renewal even after a major fire.
But obviously health care is different. Health problems this year greatly raise the probability of health problems in future years. There is every incentive for an insurer to bail on you after one bad year. This is the major fear that then follows the need - that catastrophic insurance will no longer be available after the first claim. Had health insurance developed differently (e.g. with policies that covered more than just one year, more like term life) we might be in a different situation, but here we are.
Government is Good at Having Lots of Money on Call
And the good news is that the one thing the government is really, really good at is being an insurer of last resort -- they have the deep pockets and the fiat money power to do this better than anyone else -- that is why they are the insurer of last resort of bank deposits and for flood insurance (I am not saying that there are not moral hazards in these or unintended consequences, but the insurance works). So there is the clear opportunity -- what people need most is catastrophic insurance even when the private market won't provide it and the government does really well is provide catastrophic insurance as a last resort.
Before we get into the plan itself, let's discuss a few things that the government does NOT do well:
Government is Bad at Cost control.
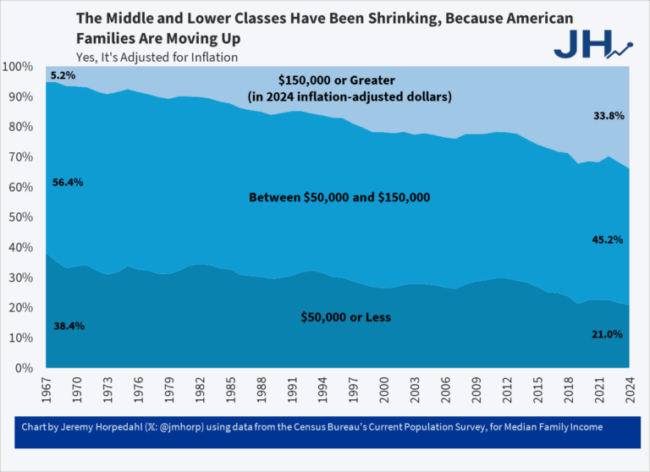
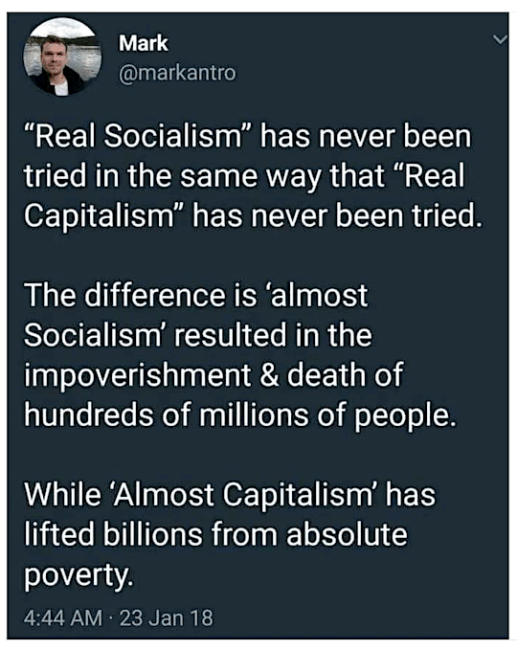
I feel like arguing that government is bad at cost control should be about as necessary as arguing that socialism always fails, but I guess it just needs to be repeated over and over. A large part of the PPACA (Obamacare) was adding provisions meant to reap cost savings in health care. None of it has worked. The problem is that any real markets for health care have been disappearing for decades as more and more health care expenses get paid by third parties rather than individuals making price/value trade-offs (as they do with pretty much everything else -- the prosaic word for this is "shopping").
Now, Democrats are increasingly seeking "single payer" health care, arguing that aggregating all purchases in one entity will result in huge negotiating leverage. But this never has been true. It is impossible to have a real price negotiation without a market, and market price, to reference. Look at another area of government spending where the government does 100% of the industry purchasing: military hardware. Do you really have the sense that the military is getting great pricing due to their purchasing power? Supporters will site discounts that Medicare gets over other buyers for certain services and pharmaceuticals. But note again that this is all in reference to a market price benchmark, that will disappear with single payer. Further, many of the savings Medicare gets are not real savings, but cross subsidies where other customers end up paying more so Medicare can get something below cost. When the government is buying everything, this cross-subsidy goes away. And can you even imagine the lobbying and cronyism and opportunities for graft that will exist once government pricing is untethered from any market price? Just think again about military procurement.
I suppose that the government could turn all health care suppliers into a huge regulated utility, for example paying pharmaceutical companies a utility-like cost plus a fixed return on drugs. If this occurs, I hope you are satisfied with the range of treatments you have today because you won't get many others -- if you don't believe me, name the three most recent innovations that have come out of your local regulated utility. Typically all they do is fight innovation (e.g. rooftop solar and co-generation).Finally, the government has a lot of regulations that Congress did not touch in the PPACA that restrict supply and greatly increase costs. For example, many states and municipalities have certificate of need processes that prevent new entrants from adding hospitals or even new equipment without the permission of existing competitors. The same is true in occupational licensing, which protects the most skilled (and expensive) health care workers from competition on simple procedures (e.g. why is someone required to go through a decade of medical training to put stitches in my kid's elbow?)
I will say that the PPACA has perhaps had an accidental effect on costs but not through any intended mechanism. As deductibles in the gold/silver/bronze exchange plans have gone up to try to keep a lid on premiums, individuals previously used to first dollar health care now find themselves responsible for making spending choices. This is a good thing, maybe the best part of the whole program.
Government is Bad at Service Effectiveness.
The PPACA also sought to increase the effectiveness of health care providers. The problem is that it is impossible for a small group of people in Washington to do this. We are 300 million consumers who each make trade-offs in different ways and define effectiveness differently. Take an example from another field: Hair care. In the state of AZ, hair cutters must go through 2000 hours of training to be licensed to cut hair -- they must demonstrate proficiency in all sorts of hair styles. I personally don't give a cr*p about that -- I tend to choose the fastest, cheapest person who does a reasonable job. But no one in government has anticipated that as a valid consumer need.
The PPACA was larded with expensive provisions that reflected the vision of a few elites about how they personally wanted health care performed. A great example is the whole electronic medical records requirement, likely stuck in their based on a lot of intensive lobbying by makers of this software. I have yet to meet a doctor who likes this software, or who feels that their patient service is improved by it, but everyone has to do it none-the-less.Perhaps even more than the cost issue, it is amazing to me that anyone believes that government involvement will make some service more effective. If you think it can, I urge you to take two identical copies of documents, and go through the process of sending and tracking one by Fedex and sending and tracking one via the post office
Outlines of A Plan
I am not sure how you actually do this, but I think being clear on the goal and the useful (and not useful) roles of government in the process are good. Rather than a plan, I offer some design goals for a plan
- Make the government the insurer of last resort to make sure that all Americans are protected against catastrophic health care costs in a year. One approach, though probably not the most compact, is to make the government responsible for all non-discretionary individual health care expenditures in a year above a certain percentage of that person's adjusted gross income for that year. I am thinking personal responsibility numbers that start at 15% of AGI and could increase in higher income brackets. Yes, if you are a person making $50,000 a year, then $7,500 of out of pocket health care expenses will be difficult -- but likely not bankrupting and not a barrier to getting needed care. Perhaps we exclude social security from AGI and apply this to seniors as well, effectively eliminating medicare and phasing out government benefits for wealthy seniors.I am open to a more compact way of doing this. Perhaps guaranteed-entry government subsidized high-risk pools for health insurance. The problem is that insurance companies will just dump all their expensive customers into those pools and we will end up with a system as costly to the taxpayers as the one above but less rationally organized.
- Shift as many of the individual spending price / value tradeoffs as possible into individual hands. The step outlined above in #1 is a good start, at least for more routine purchases. As a design goal, at every turn, try to build in ways for consumers to get money back or get rewarded for choices to use less or more inexpensive care.I do not think there is anything with more potential leverage for improving the health care world than bringing back individual shopping for medical care. My kid used to injure himself a lot in sports and we had a high deductible on our insurance, so we found a sports medicine guy who charged us only $50 a visit if we paid cash. Then he told us that when we went downstairs to the radiology company, to tell them we were paying cash. Sure enough, the lady there pulled out a special book from behind the counter and the $300+ they charge to the insurance companies became $40 to us. On the other hand, we have spent weeks talking to doctors and hospitals about heart surgery my mother-in-law (who is covered by Medicare) needs. You know what has not come up a single time? Price. I have zero idea how much it will cost -- but let's say it is $100,000. Can you imagine buying anything else that expensive without discussing the price once?
- Any medical benefits paid by the employer become fully taxable
- Price transparency mandates -- every provider must disclose the best price it sells a product and service at, as well as your price. For all but emergency procedures, a cost estimate must be given in advance (My dog had to have surgery and even in an emergency condition they gave me a detailed cost estimate in advance).
- Systematic review of supply restrictions and rethinking of licensing arrangements. Banning of state and local certificate of need processes.
- Accelerated and streamlined drug approval process. Really what I would like to see is that there is a government led testing process that leads not to an approval/refusal but to the publication of safety/effectiveness data that doctors and patients can then use to make their own decisions.
Hat tip to Megan McArdle who has been suggesting something like this for years, probably long before I started thinking about it.